Northwestern Medicine shares new findings from the Comprehensive COVID-19 Center as significant demand remains for patient appointments
A new study published in the American Journal of Medicine reports key findings from more than 1,800 patients who were evaluated during the first 21 months at the Northwestern Medicine Comprehensive COVID-19 Center with neurology, pulmonology and cardiology being the most commonly accessed specialties and still in high-demand today.

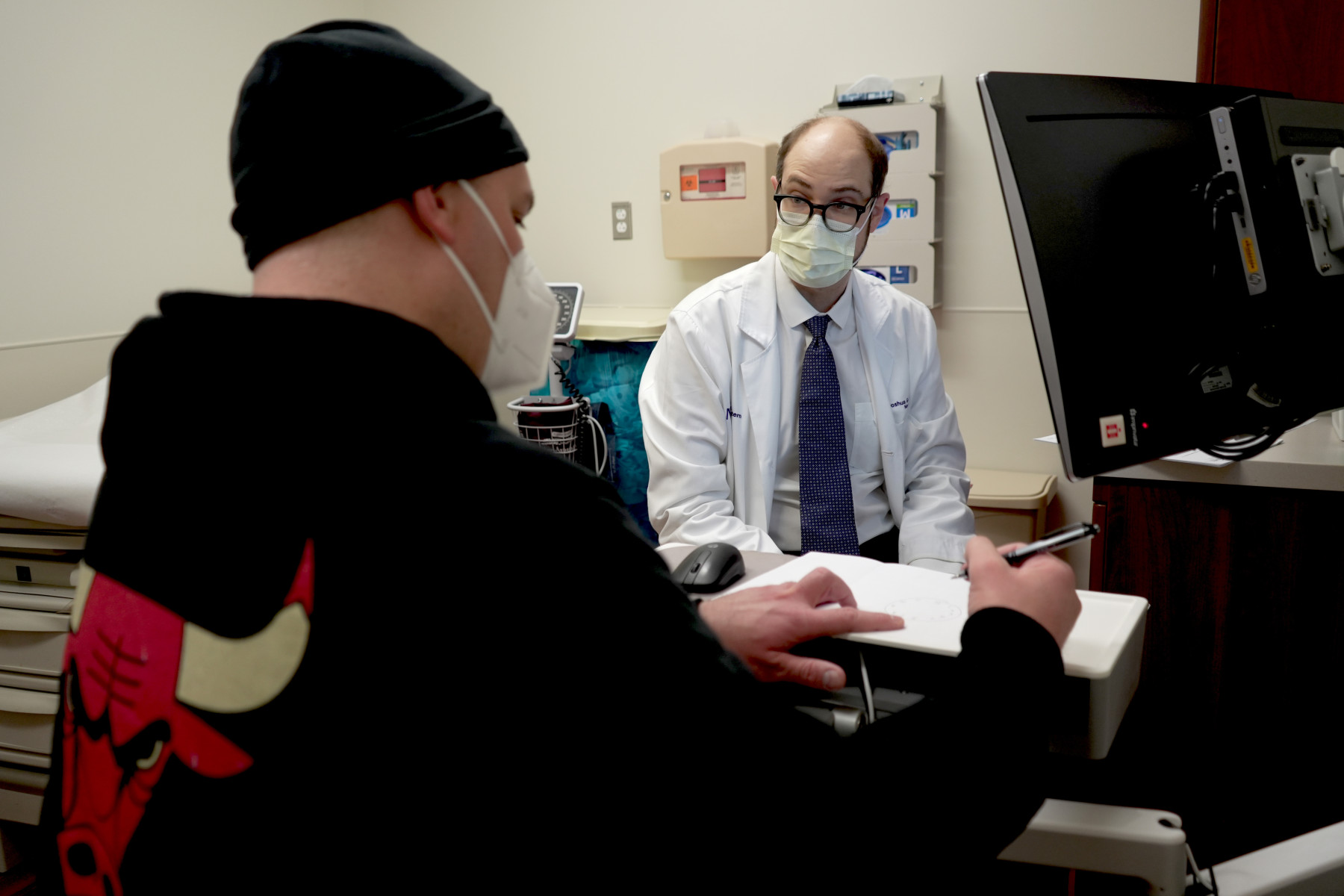
CHICAGO – July 13, 2023 – Long COVID occurs in approximately a third of COVID survivors and is now the third leading neurologic disorder in the United States. In May 2020, during the height of the pandemic, Northwestern Medicine physicians noticed this growing trend and established one of the first Comprehensive COVID-19 Centers in the United States to treat patients suffering from lingering impacts of the virus such as brain fog, shortness of breath and chest pain. Three years later, a new study published in the American Journal of Medicine reports key findings from more than 1,800 patients who were evaluated during the first 21 months at the Northwestern Medicine Comprehensive COVID-19 Center (CCC) with neurology, pulmonology and cardiology being the most commonly accessed specialties and still in high-demand today.
“The COVID-19 public health emergency may be over, but the need for long COVID care still remains. To date, we’ve treated nearly 4,000 patients from 44 states at the CCC, and our team of 42 clinicians continue to see approximately 100 patients each month,” said Igor Koralnik, MD, chief of neuroinfectious diseases and global neurology at Northwestern Medicine, who is co-director of the Comprehensive COVID-19 Center. “The disease burden of long COVID continues to grow in this country with significant implications for the economy and population health.”
“Due to widespread vaccination, rates of acute COVID infection have decreased significantly, however, millions of patients are still suffering from persistent symptoms that may have occurred years ago,” said Marc Sala, MD, pulmonary and critical care specialist at Northwestern Medicine, who is co-director of the Comprehensive COVID-19 Center. “To date, little is known about the characteristics and outcomes of patients seeking care at multidisciplinary post-COVID centers and the approach to caring for these patients widely varies among institutions and providers. This study will help us understand what the biological causes of those symptoms are and how to structure clinics to care for them.”
KEY FINDINGS
The team evaluated 1,802 patients (350 post-hospitalization and 1,452 non-hospitalized) via telehealth or in-person at the CCC between May 2020 and February 2022. Patients were seen in 2,361 initial visits in 12 specialty clinics including neurology, pulmonology, cardiology, otolaryngology, gastroenterology, infectious diseases, endocrinology, nephrology, hematology, dermatology, psychiatry and rheumatology. Patients most commonly sought treatment from neurology (49%), pulmonology (25%) and cardiology (12%) specialists.
Among patients tested:
- 85% of patients reported decreased quality of life
- 51% had cognitive impairment
- 45% had altered lung function
- 83% had abnormal CT chest scans
- 12% had elevated heart rate on rhythm monitoring
- Frequency of cognitive impairment and pulmonary dysfunction was associated with severity of acute COVID-19
- Non-hospitalized patients with positive COVID-19 testing had similar findings than those with negative or no test results
DEMOGRAPHICS
- 65% of patients identified as female
- Average age at first clinic visit was 47 years old
- 72% were White, 10% were Black, 4% were Asian and 13% were Hispanic

“The population predominantly consisted of females in their forties, and our data shows that critically ill, hospitalized, and non-hospitalized patients have distinct neurologic, pulmonary and cardiac manifestations of long COVID, which should be studied and treated differently,” said Joseph Bailey, MD, pulmonary and critical care specialist at Northwestern Medicine, who treats patients in the CCC.
“One of the key findings of this study is that there is a very wide range of long COVID manifestations that depend largely on the severity of acute COVID-19 illness, and that they can’t be treated with a ‘one size fits all’ approach,” said Dr. Koralnik. “Some patients who had severe COVID-19 may have sustained permanent organ damage, while persistent symptoms in those with mild initial disease may be caused by different mechanisms. This requires an individualized, precision medicine approach to long COVID care.”
“There is a great need for multidisciplinary clinics to form the backbone of the response to long COVID. With multiple clinicians caring for and evaluating patients under the same roof, multidisciplinary long COVID clinics can recognize and respond to different presentations and manifestations of long COVID more quickly than other care models,” added Dr. Sala. “This study is the first to show the impact of a multidisciplinary effort and could be an example for use in future viral outbreaks.”
For more information on the CCC, visit nm.org and to schedule an appointment, please call 312.926.9900.
Contact

|
Jenny Nowatzke Manager, National Media Relations - Northwestern Memorial Hospital 312.926.2131 |
